10th Edition of
World Congress on Infectious Diseases & One Health
October 05-07, 2026 | Tokyo, Japan
Another significant category of intravascular infections is infective endocarditis (IE), which involves the inflammation of the inner lining of the heart chambers and valves. Endocarditis often results from the colonization of heart valves by microorganisms, typically bacteria, entering the bloodstream. Predisposing factors include pre-existing heart valve abnormalities, intravenous drug use, and certain medical procedures that introduce bacteria into the bloodstream. The pathogenesis of infective endocarditis involves the adherence of microorganisms to damaged heart valves, leading to the formation of vegetations composed of bacteria, fibrin, and platelets. These vegetations can embolize, causing systemic complications such as septic emboli in various organs. Common causative agents of infective endocarditis include Staphylococcus aureus, Streptococcus viridans, and Enterococcus species. Diagnosis is challenging and often requires a combination of blood cultures, echocardiography, and clinical criteria. Treatment involves prolonged courses of intravenous antibiotics tailored to the identified pathogens. Surgical intervention, such as valve replacement, may be necessary in severe cases or when complications arise. Prevention of infective endocarditis involves antibiotic prophylaxis before certain dental and medical procedures in individuals with high-risk cardiac conditions.
By signing up, you agree to join our mailing list to receive information and updates.
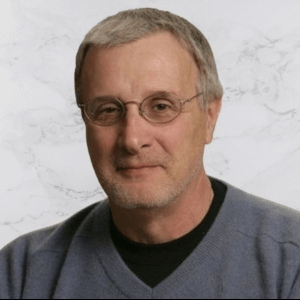
Title : Molecular crosstalk between the host and pathogen in Streptococcus pyogenes virulence
Francis J Castellino, University of Notre Dame, United States
Title : The impact of expanded adolescent vaccination against Omicron waves depends on the epidemic status: A mathematical modelling study
Anna Fairweather, University of Oxford, United Kingdom
Title : Comprehensive HIV care through integrated STI and primary care services at the LGBTQ+ Center of Southern Nevada
Darya V Fridman, The Southern Nevada LGBTQ+ Center, United States
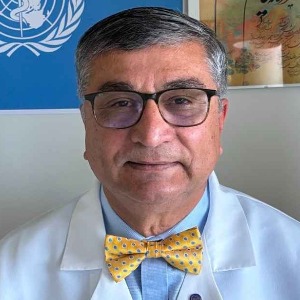
Title : Host brakes on viral inflammation
Saurabh Chattopadhyay, University of Kentucky College of Medicine, United States
Title : Meeting the needs of adults aged 50+ with HIV through the new opening of a primary care clinic at the LGBTQ Center of Southern Nevada
Darya V Fridman, The Southern Nevada LGBTQ+ Center, United States
Title : Common infections in cancer patients – narrative review and clinical pearls
Patricia Tai, University of Saskatchewan, Canada