10th Edition of
World Congress on Infectious Diseases & One Health
October 05-07, 2026 | Tokyo, Japan
The intricate mechanisms of action of beta-lactam antibiotics make them a cornerstone in the fight against bacterial infections. The fundamental principle lies in disrupting bacterial cell wall synthesis, an essential process for bacterial survival. Penicillin-binding proteins (PBPs), located on the bacterial cell membrane, are the primary targets of beta-lactam antibiotics. These antibiotics mimic the structure of D-alanyl-D-alanine, a substrate for the transpeptidation reaction during peptidoglycan synthesis. By binding irreversibly to PBPs, beta-lactam antibiotics prevent the cross-linking of peptidoglycan strands, leading to weakened cell walls and eventual cell lysis. Despite their success, bacterial resistance to beta-lactam antibiotics has emerged as a significant concern. One of the main mechanisms involves the production of beta-lactamase enzymes, which cleave the beta-lactam ring, rendering the antibiotic ineffective. To counteract this, scientists have developed beta-lactamase inhibitors, such as clavulanic acid, which are often combined with beta-lactam antibiotics to enhance their efficacy. Additionally, bacteria may alter or reduce the expression of PBPs, limiting the binding sites for beta-lactam antibiotics. Understanding these resistance mechanisms is crucial for designing new generations of beta-lactam antibiotics and developing strategies to combat bacterial infections effectively. Ongoing research in this field aims to stay ahead of evolving resistance patterns and ensure the continued success of beta-lactam antibiotics in the clinical setting.
By signing up, you agree to join our mailing list to receive information and updates.
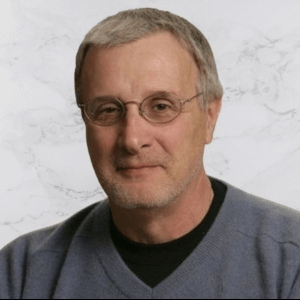
Title : Molecular crosstalk between the host and pathogen in Streptococcus pyogenes virulence
Francis J Castellino, University of Notre Dame, United States
Title : The impact of expanded adolescent vaccination against Omicron waves depends on the epidemic status: A mathematical modelling study
Anna Fairweather, University of Oxford, United Kingdom
Title : Comprehensive HIV care through integrated STI and primary care services at the LGBTQ+ Center of Southern Nevada
Darya V Fridman, The Southern Nevada LGBTQ+ Center, United States
Title : Host brakes on viral inflammation
Saurabh Chattopadhyay, University of Kentucky College of Medicine, United States
Title : Meeting the needs of adults aged 50+ with HIV through the new opening of a primary care clinic at the LGBTQ Center of Southern Nevada
Darya V Fridman, The Southern Nevada LGBTQ+ Center, United States
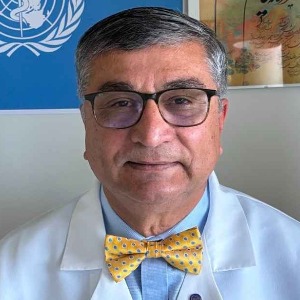
Title : Common infections in cancer patients – narrative review and clinical pearls
Patricia Tai, University of Saskatchewan, Canada